Guidelines for Pulmonary Rehabilitation in TB [Draft]
Guidelines for Pulmonary Rehabilitation in TB [Draft]
Guidance Document on Pulmonary Rehabilitation for People affected with Tuberculosis at Rajan Babu Institute of Pulmonary Medicine and Tuberculosis (RBIPMT), Delhi 2024.
This work is available under the Creative Commons Attribution-NonCommercial-3.0 IGO license (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this license, you may copy, redistribute, and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. The use of the logos provided in this document is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons license. Any mediation relating to disputes arising under the license shall be conducted in accordance with the mediation rules of the Government of India.
Suggested citation: Guidance Document Pulmonary Rehabilitation for People affected with Tuberculosis at Rajan Babu Institute of Pulmonary Medicine and Tuberculosis (RBIPMT), Delhi 2024.
Cataloging-in-Publication (CIP) data: Contributor author: RBIPMT, Delhi; Coverage spatial: New Delhi, India; Date issued: July 2024; Language: English; Rights: CC BY-NC-SA 3.0 IGO;
To submit requests and queries on rights and licensing, write to: director-rbipmt@mcd.nic.in
General Disclaimer: All reasonable precautions have been taken by the RBIPMT, Delhi to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The purpose of this document is to provide guidance on how to integrate pulmonary rehabilitation in TB care at DR-TB centres and is not legally binding. The responsibility for the interpretation and uses of the material lies with the reader.
Live Document: Due to the evolving nature of the program the guidelines need to be updated frequently in accordance with it. This would mean that the content would be updated as and when any policy, procedure or technical instructions are changed.
Acknowledgement
AcknowledgementThe Guidance Document for Pulmonary Rehabilitation Programme for People affected with Tuberculosis at Rajan Babu Institute of Pulmonary Medicine and Tuberculosis is an initiative by Central TB Division (CTD) and Rajan Babu Institute of Pulmonary Medicine and Tuberculosis (RBIPMT), New Delhi, the Center of Excellence for DR-TB care. The guidelines have been developed as the end product of series of consultations and meetings of the working committee held under the chairperson of Dr Manasi Anand, Director RBIPMT.
The work on this document was guided and supported by Dr Sanjay Kumar Mattoo, Joint Commissioner and Addl DDG (TB), CTD. We would also like to acknowledge Dr Malik Parmar (NPO, WHO India), Dr Jyoti Jaju (Director Programmes, The Union), Dr Bhavin Vadera (Senior Health Advisor, USAID), Dr Sandeep Chauhan (National Consultant, CTD) and Dr. Manu Mathew (Deputy Director Programmes) for their guidance. We also acknowledge USAID supported The Union led iDEFEAT TB Project for co-ordination and technical assistance.
We express our gratitude to the eminent technical experts involved in the development of the document (alphabetical Order) Dr Anuj Bhatnagar (Head Department of Respiratory Medicine, RBIPMT), Dr Anil Choudhary (Senior Pulmonologist, RBIPMT), Dr Ashwani Khanna (NTEP Advisor, Delhi), Dr B.K Vashishat (STO, Delhi), Dr Bhoomika Varshney (Department of Yoga, RBIPMT), Dr Rakesh Kumar (Physiotherapist, RBIPMT), Dr Rakesh P.S (Senior Technical Advisor, The Union), Dr. Sanjeev Nair (Government Medical College, Thrissur), Dr Shruti Sasastrabudhe (Symbiosis, Pune), Dr Sunalini Saini (Senior Physiotherapist, RBIPMT) Dr Sunita Kujur (CMO, RBIPMT), Dr Vishal Bansal (Vallabhbhai Patel Chest Institute, Delhi), Dr Vaishali (Dietician, RBIPMT), and Dr Yatin Dholakia (Medical Research, Mumbai). Writing of the document was coordinated by Dr Priyanka Bindroo (Former National Consultant, CTD), Dr Meera Bhatia (Technical Advisor, The Union) and Dr Mayank Mittal (National Consultant, CTD).
Acronyms
Acronyms| AFB | Acid fast Bacilli |
| AIC | Airborne Infection Control |
| BMI | Body Mass Index |
|
CPR |
Cardio- pulmonary Resuscitation |
|
COPD |
Chronic Obstructive Pulmonary Disease |
|
CTD |
Central TB Division |
|
HRQoL |
Health related Quality of Life |
|
6MWT |
6- minute Walk Test |
|
mMRC scale |
Modified Medical Research Council Scale |
|
PRC |
Pulmonary Rehabilitation Centre |
|
SoP |
Standard of Procedures |
|
SGRQ |
St. George’s respiratory Questionnaire |
|
TB |
Tuberculosis |
|
UVGI |
Ultra-violet Germicidal Irradiation |
Background
BackgroundTuberculosis is a major contributor to the pool of individuals who have respiratory insufficiency due to destruction of lung tissue. It has been shown that 65% of patients completing their TB treatment have abnormal lung functions and residual symptoms.
Pulmonary rehabilitation aims to restore the affected individual to an independent, productive and lead a satisfying life and prevent further clinical deterioration to the maximum extent compatible with the stage of the disease. This goal may be accomplished, without materially improving lung function, by helping the patients to become more aware of their disease, more actively involved in their own health care and more independent in performing daily care activities, attempting to reverse the disability from disease.
Pulmonary rehabilitation is a comprehensive intervention, based on a thorough patient assessment followed by patient-tailored therapies, that include but are not limited to exercise training, education and behaviour change. It is designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence to health-enhancing behaviours. Pulmonary rehabilitation provided to individuals with chronic respiratory diseases other than COPD (i.e., interstitial lung disease, bronchiectasis, cystic fibrosis, asthma, pulmonary hypertension, lung cancer, lung volume reduction surgery, and lung transplantation) has demonstrated improvements in symptoms, exercise tolerance, and quality of life. This effort is in the direction to incorporate rehabilitation early in the management of tuberculosis so that the patients in addition to being cured are holistically managed.
USAID India funded, and The Union led iDEFEAT project is supporting the CoE RBIPMT, New Delhi in establishing a centre of excellence in pulmonary rehabilitation for people affected with TB. The purpose of this SOP is to integrate pulmonary rehabilitation in the standard of care for individuals with TB, with a specific focus on improving overall well-being of the affected individual. This document will be a guide to all healthcare professionals, including physicians, nurses, physical therapists, and other staff involved in the care and rehabilitation of patients with TB as well as chronic respiratory diseases.
The aims of pulmonary rehabilitation are:
- Decrease of physical and psychological impairment due to the disease
- Increase in physical and mental fitness and performance
- Maximal social reintegration of the patient and self-sufficiency.
Pulmonary rehabilitation is implemented by a dedicated, interdisciplinary team including physicians/health care professionals, physiotherapists/respiratory therapists, nurses, psychologists, nutritionists, occupational therapists, and social workers. The intervention should be individualized to the unique needs of the patient, based on initial and ongoing assessments, including disease severity, complexity, and comorbidities. Although pulmonary rehabilitation is a defined intervention, its components should be integrated throughout the clinical course of a patient’s disease. Pulmonary rehabilitation may be initiated at any stage of the illness. The programme is good for one-to-one guidance, but group exercises can be incorporated on the need basis.
Infrastructure
InfrastructureInfrastructure
The Pulmonary Rehabilitation Centre (PRC) should be located in or close to a hospital.
To set up a dedicated pulmonary rehabilitation unit the following are the basic requirements:
-
An independent space with good ventilation (6-12 Air Change per Hour).
-
Area of 1000 square feet (20 x 50 feet room). This space will house the clinic room, counselling, physiotherapy section, data management and other facilities.
-
A corridor 30-35 meters, non-slippery, free from movement of people, fitted with hand rails on either side and also with oxygen ports and chairs alongside.
-
Area for hand washing/washroom.
Equipment
EquipmentIn order to establish a pulmonary rehabilitation unit, the following equipment are required.
|
Essential |
Desirable |
||
|
Equipment name |
Quantity |
Equipment name |
Quantity |
|
Treadmills |
1 |
Inspiratory muscle trainer |
1 |
|
Recumbent bicycles |
1 |
High flow oxygen/ BiPAP |
1 |
|
Trolley |
1 |
Stop watch |
1 |
|
Oxygen supply (wall mounts/ oxygen cylinders/ portable light weight) |
2 to 3 |
Equipment to measure Fat Free Mass |
1 |
|
Wheel chair |
1 |
Aerobic stepper |
1 |
|
Hand Ergometers |
1 |
Big ball |
1 |
|
Air bikes |
1 |
Thera bands |
1 |
|
Steps |
1 |
Oximisers |
2 |
|
Spirometer |
1 |
Rollators |
2 |
|
Nebuliser |
1 |
AED/ Defibrillator |
1 |
|
Weighing machine |
1 |
LCD with screen |
1 |
|
Pulse oximeter |
1 |
|
|
|
Nasal cannulas |
2 to 3 |
UPS / power backup supply |
|
|
Masks (surgical/N-95) |
Need based |
|
|
|
Tilt table |
2 |
|
|
|
Crash cart with essentials |
1 |
|
|
|
Power and electric connections and points |
8 (Minimum) |
|
|
|
Free-weights (dumbells + ankle cuffs) |
|
|
|
|
0.5 kgs,1 kg, 1.5 kg, 2kg, 3kg |
1 each |
|
|
Human Resource
Human ResourceIn order to get the pulmonary rehabilitation programme running at any site, the following are the required personnel:
-
One Doctor
-
One Nurse
-
Two Physiotherapists
-
One Yoga trainer (Desirable)
-
One Dietician
- One Psychologist (Desirable)
- One Scheduler/ recording person/ an administrative person/ nurse (can be an asset in case of any female patient)
- One helper/ orderly person
Pulmonary Rehabilitation Programme
Pulmonary Rehabilitation Programme RichardSEligibility, referral and assessment
Eligibility, referral and assessment-
Eligibility Criteria
People with tuberculosis need to be identified, assessed and referred to the pulmonary rehabilitation programme. The Medical officer at the PHC/Health and Wellness Centre or the chest clinics shall identify people affected with tuberculosis and on basis of the following to refer the candidate to the pulmonary rehabilitation programme.
Inclusion criteria
- Patients who have dyspnoea or cough due to Tuberculosis
- Patients with post TB fibrosis, pleural thickening, bronchiectasis, with fibro-cavitary lesions or with destroyed lungs diagnosed on basis of Radiology (X-Ray/ CT scan)
- Reduced exercise tolerance
- People with post tubercular obstructive airway disease diagnosed clinically or on spirometry
- People on treatment needing support with issues like psychosocial support/ de-addiction/ alcoholism/ smoking cessation
Exclusion criteria
- People who are unable to walk or having locomotor issues
- People who have unstable angina or have had recent myocardial infarction or having unstable heart diseases like
- People having difficulties following instructions due to cognitive or psychiatric impairments
- People with uncontrolled Blood Pressures, Diabetes, liver diseases, low haemoglobin levels or low oxygen saturations (<80%).
Pulmonary rehabilitation programme will benefit individuals who have completed treatment for tuberculosis or are on treatment as per the above mentioned inclusion/exclusion criteria. These include:
- Out-patients
- Immobile or in-bed patients, where the pulmonary rehabilitation programme can be offered near the bedside
- In-patients who can attend the pulmonary rehabilitation programme at the centre and come back post discharge to complete 3 months of the program
2. Referral for Pulmonary Rehabilitation
The doctors at DR-TB center/ chest clinics/ peripheral health institutes should carefully evaluate every case of pulmonary TB completing treatment for the possibility of developing Post TB Lung Disease and then refer them to the pulmonary rehabilitation programme centre. The assessment should be conducted at the earliest and at the end of treatment. Basic examinations should be conducted with the aim to identify patients with sequelae at risk of deterioration and those likely to benefit from Pulmonary rehabilitation program.
The following set of basic examinations is considered essential before referral to a pulmonary rehabilitation program:
- Clinical examination and brief medical history
- Persistent symptoms
- Dyspnoea/breathlessness
- Disability of daily activities
- Sputum examination: smear / culture
- Chest X-Ray
- Spirometry
- Six-minute walk test (6MWT)
3. Patient assessment at Pulmonary Rehabilitation Centre
The patients will be enrolled on Pulmonary Rehabilitation Programs based on the clinician's referrals and indications for rehabilitation. Following this, they will be undergoing education and counselling regarding the importance of pulmonary rehabilitation and how it will affect their quality of life.
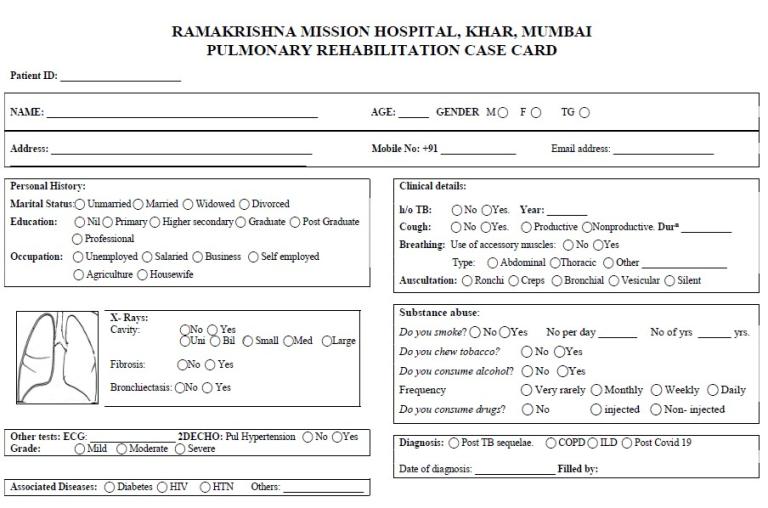
The patient card will be completely filled up with all the below mentioned. (patient card is depicted in Annex 4)
- Detailed and complete medical history of the person to be recorded
- Complete baseline clinical examination to be conducted
- Assessment of quality of life using St. George questionnaire (Annex 1)
- Assessment of dyspnoea using modified MRC scale (Annex 2)
- Height, weight, Body Mass Index
- Hb% (Haemoglobin levels)
- Blood sugar levels- Fasting & Post prandial
- Pulmonary Function Test results
- X-Ray chest PA view
- Sputum for AFB
- ECG
- 6-minute walking test result with SpO2 levels (Annex 3)
|
Parameters |
Methods of assessment |
|
Impaired exercise capacity |
Six-minute walking test (Annex 3) Five repetitions sit to stand test |
|
Impaired pulmonary function showing airflow obstruction or restriction or mixed abnormalities and bronchodilator response |
Spirometry |
|
Impaired quality of life |
Modified Medical Research Council scale (Annex 2) |
Respiratory Therapy
Respiratory TherapyAfter the enrolment there is a plan designed for the individual. This person-tailored nature of pulmonary rehabilitation, means that the desirable components of pulmonary rehabilitation should vary across individuals according to their needs suiting to their needs and in a manner most convenient to them.
The rehabilitation sessions include breathing exercises, airway clearance techniques, thoracic mobility exercises, posture correction and incentive spirometry. It also includes teaching them energy conservation techniques such as planning, prioritising the activities, pacing, and use of proper body mechanics.
Breathing and Exercise training
Breathing and Exercise trainingBased on the number enrolled, it could be given in a group of 5 people. If there are 30 members enrolled, they may be divided into 6 groups of 5 each.
- Each group may be advised a pulmonary rehabilitation program for duration of 6-12 weeks.
- There should be 3 supervised sessions per week
- A warm up session of 5-10 minutes prior to the session and a cool down-stretching session 5 minutes’ post exercise session is recommended.
a. Airway clearance techniques:
Choose the technique suitable for the subject among those available, based on respiratory capacity, mucus rheology, and patient preferences.
- 15–30 min one or more times/day.
- Choose the duration of treatment based on chronicity
- Suggest maintenance programme when needed
b. Breathing Exercises:
Teach the patients the mentioned techniques which will aid them in breathing in an efficient manner with all the reserves they are left with.
- Pursed lip Breathing
- Deep diaphragmatic Breathing
- Incentive Spirometer
- Postural Drainage Positions
-
Huffing/ Coughing Techniques
c. Inspiratory muscle training:
- Load threshold devices are used with patient seated and using a nose clip.
- It is an interval training where 10 exercises sets are followed with 10 seconds break between each training
d. Aerobic exercise:
Endurance training
Each person performs the following exercises in rotation
- Treadmill
- Arm ergometry
- Walking
- Stepping
- Stationary cycling
Time duration for each exercise should be in bouts of 10 minutes each and the frequency should be minimum of 3 and up to 5 times a week for 4–8 weeks. The intensity to be set according to the perceived dyspnoea.
e. Strength training:
The following sets of exercises should be carried out in sets of 2-3 with 6-12 repetitions. The frequency of the regimen be 3 days in a week with the duration of session being 20-30 minutes. Intensity set according to perceived muscles fatigue. Free weights (dumbbells and ankle-brace) can be used.
Upper limb:
- Shoulder forward flexion
- Shoulder abduction
- Overhead shoulder press
- Biceps curl
- Overhead triceps extension
- Scapular retraction
Lower limb:
- Wall squats
- Lunges
- Hip abduction
- Hip extension
- Dynamic quads
- Calf raises
Yoga training
Yoga trainingThe pulmonary rehabilitation program should incorporate the yoga session as per the individualized plan wherever there is availability of trained yoga teachers/ instructors under their expert guidance.
Pharmacological management of comorbidities
Pharmacological management of comorbiditiesSome of the entities to be kept in consideration during the program or while preparing the discharge/ follow up card are as follows:
- Desaturation: Start oxygen by nasal cannula/ mask
Use oxymizers if patient is on oxygen therapy
- Breathlessness: Nebulize with Bronchodilators/ Inhaled steroids
Intravenous injection of Hydrocortisone/ Deriphyllin
- Haemoptysis: Intravenous injection of Tranexamic acid
Nebulization with Adrenaline
- Acute cardiac event/ unconsciousness: Perform CPR, call for an ambulance with medical assistance and shift to hospital
- Diabetes: Check for their regular medicine adherence/ check for control/ educate on importance of control
- Hypertension: Check for their regular medicine adherence/ check for control/ educate on importance of control
- Hypothyroidism: Check for their regular medicine adherence/ check for control/ educate on importance of control
- Patient on regular use of INHALERS with inhaled steroids/ bronchodilators, check for the techniques
Nutritional support
Nutritional supportFor every person enrolled in the pulmonary rehabilitation program
- Nutritional assessment should be carried out.
- Evaluate and address malnutrition by education on a balanced diet rich in nutrients.
- Monitor weight and dietary intake regularly.
Psychological support
Psychological supportFor every person enrolled in the pulmonary rehabilitation program
- Psychological assessment to be carried out
- Psychological support to be provided through personal counselling, counselling of family members.
- Smoking & Alcohol cessation linkages and services to be strengthened
Follow-up visits
Follow-up visitsThe follow-up sessions will focus on maintaining the effects achieved and the progress made. It will be based on the improvement in patient-reported outcome measures and the patient's signs and symptoms and vital parameters.
-
At the end of 12 sessions, information on patient experience, needs and satisfaction, during and after the pulmonary rehabilitation to be collected and recorded.
-
The clients to be provided with a comprehensive discharge plan, including medication instructions and follow-up appointments.
-
The follow up sessions to be planned every month and will be assessed on basis of the discharge plan
-
On basis of the outcome of the pulmonary rehabilitation programme help the client in beneficial vocational training
Patient Education
Patient EducationDuring the pulmonary rehabilitation programme sessions, group talks should be arranged to educate the participants on the importance and benefits of the pulmonary rehabilitation programme. The information may be imparted through visuals using the LCD screen or televisions, through group talks or individual counselling. Education should focus on:
a. TB:
- Educate clients about TB transmission, prevention, and the importance of medication adherence including avoidance of irritants
- Educate the clients about the possible adverse reactions to the drugs and also about the importance to inform the same to the treatment supervisors.
- Educate them on the importance of having a balanced diet
b. Self-Management:
- Teach the clients self-monitoring of symptoms, exacerbation recognition and when to contact the health care provider
- Teach them proper use of prescribed inhalers or respiratory devices
- Teach them technique of postural drainage in case of the post treatment sequalae
- Educate them on hazards of smoking, drinking or tobacco consumption in any form
- Importance of motivating oneself and encouraging them for vocational training
- Use of meditation and yoga in daily regime
Infection control
Infection controlIt is important to maintain a safe and healthy environment for our clients and staff and so infection control needs to be an essential aspect of our daily operations. It is crucial that we remain vigilant and proactive in preventing the spread of infection. There are some points to be kept in mind when we are running pulmonary rehabilitation unit like:
- Adherence to Air borne infection control guidelines needs to be followed.
- Regular screening of participants for viral infections and if required give them a break from the pulmonary rehabilitation programme till they recover acceptably.
- Protective equipment for the working staff as per the programmatic guidelines should be provided
- Emphasize strict hand hygiene for healthcare workers and visitors
- Adequate windows and doors should be there in the facility ensuring cross ventilation.
- In case of inadequate cross ventilation, adequate fans and exhaust fans should be there and in working condition to ensure adequate air changes per hour. UVGI as per the requirement also depending of the facility may be made available.
- Equipment sterilization techniques like use of UV towers that can be linked to the mobile Apps.
Documentation
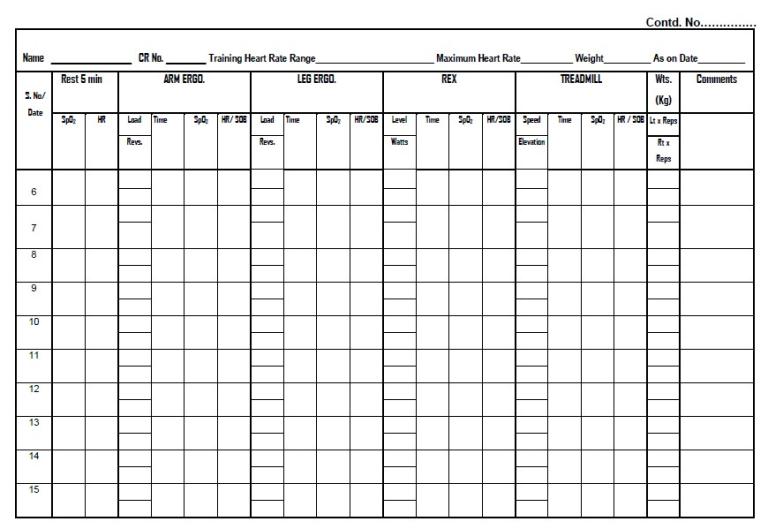
DocumentationDocumentation should be done on a paper-based format as it makes it easier for the people involved to compare and evaluate the data from different visits of the clients. It includes:
- Patient card/ discharge card
- Diary for record keeping
- Registers
- Excel sheet (electronic mode)
Monitoring and Evaluation
Monitoring and EvaluationThe following indicators may be used to evaluate the progress made by the pulmonary rehabilitation programme:
- (a). Number of people eligible for Pulmonary Rehabilitation Program
- (b). Out of (a), proportion of people took / enrolled in Pulmonary Rehabilitation Program
- (c) Out of (b), proportion of people completed Pulmonary Rehabilitation Program
- (d). Out of (c), proportion of people with an improved outcome.
Outcomes of individual clients may be documented as follows:
|
Outcomes |
Measure |
|
Lung function |
Spirometry (FEV1, FVC, FEV1/FVC) |
|
Exercise capacity |
6MWT 5STS |
|
Gas transfer |
Pulse oximetry (SpO2, % desaturation) |
|
Health-related quality of life |
mMRC score St George Questionnaire |
Annexures
Annexures RichardSComments
- Log in to post comments
India Innovation Summit: Registration Form
India Innovation Summit: Registration Form WebadminSGRQ
SGRQ RichardSMRC scale
MRC scale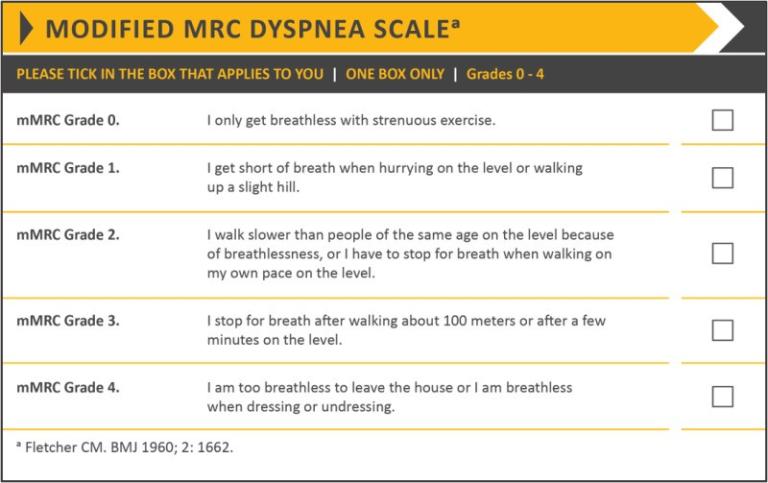
Patient card
Patient card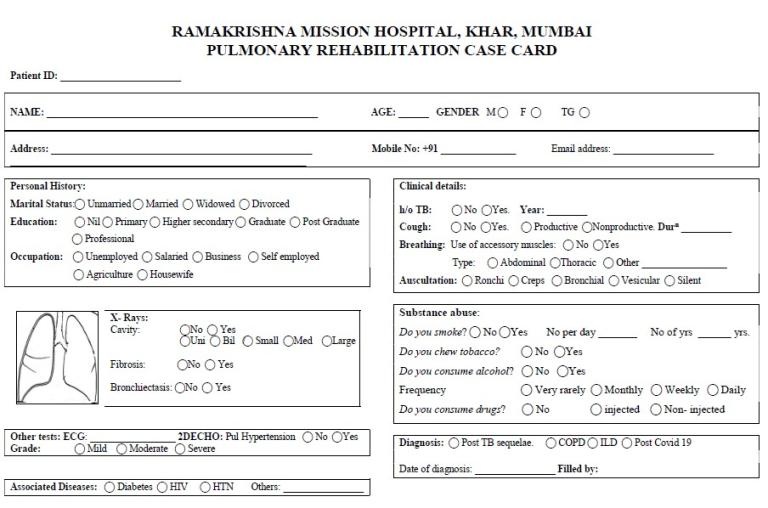
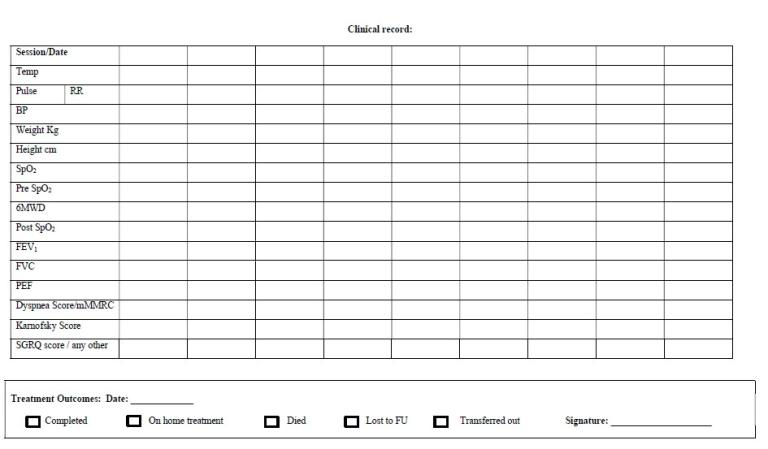
Card to record 6 minutes-walk test of the patient
Card to record 6 minutes-walk test of the patient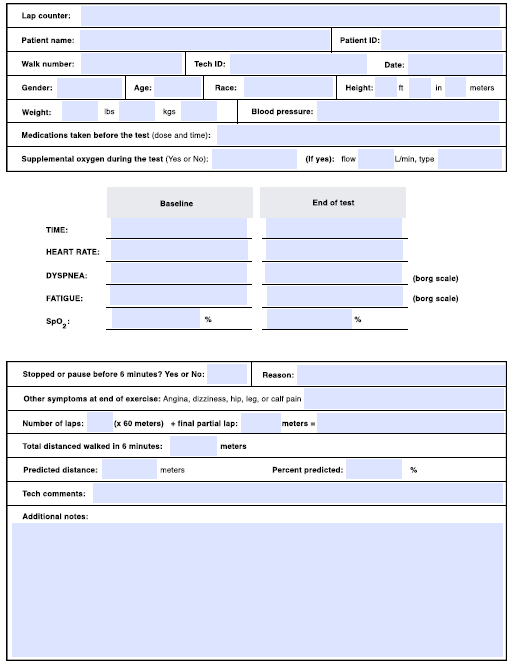
Activity Record
Activity Record
References
References-
V.V. Banu Rekha, Rajeswari Ramachandran, K.V. Kuppu Rao, et al. Assessment of long-term status of sputum positive pulmonary tb Patients successfully treated with short course chemotherapy. Ind J Tub 2009; 132-40.
-
A D Harries et al. Successfully treated but not fit for purpose: paying attention to chronic lung impairment after TB treatment. INT J TUBERC LUNG DIS 20(8):1010–1013
-
Singh S K, Naaraayan A, Acharya P, et al. Pulmonary Rehabilitation in Patients with Chronic Lung Impairment from Pulmonary Tuberculosis. Cureus. 2018; 10(11): e3664.
-
Krishan Gupta, Raj Kumar and S.N. Gaur. Effect of a Domiciliary Pulmonary Rehabilitation Programme on Disability in Patients with Interstitial Lung Diseases. Ind J Chest Dis Allied Sc.
-
Dr. Yatin Dholakia. Forum. Indian J Tuberc 2010; 57:57
-
Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. C.F. Donner, P. Howard. Pulmonary rehabilitation In chronic obstructive pulmonary disease (COPD) with recommendations for Its use. Working Group Report. Eur Reaplr J 1992, 5, 266-275