Content Status
Type
Linked Node
Screening among Household Contacts of DR-TB Patients
Learning Objectives- Understand the significance of screening household contacts of drug-resistant tuberculosis (DR-TB) patients for early detection and prevention of transmission.
- Identify the appropriate screening methods and tools for household contacts, including symptom screening, tuberculin skin testing (TST), interferon-gamma release assays (IGRAs), and chest radiography.
- Learn the importance of timely initiation of screening and follow-up procedures for household contacts.
The National TB Elimination Programme (NTEP) follows an integrated algorithm for screening and ruling out active Tuberculosis (TB) among Household Contact persons (HHCs) of Drug-resistant Tuberculosis (DR-TB) patients.
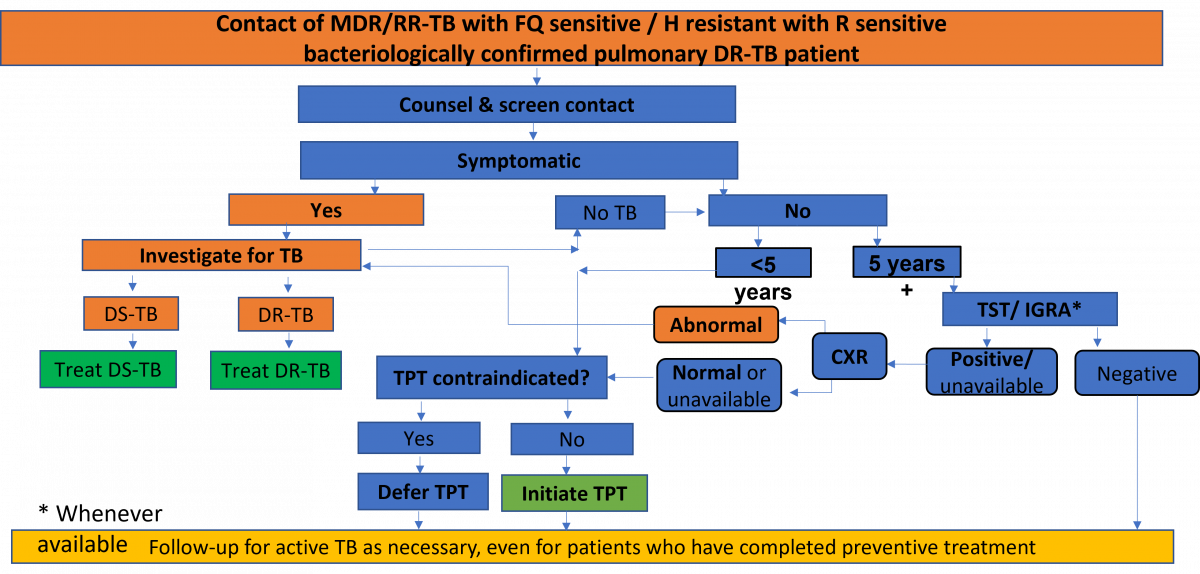
Figure: Integrated Algorithm for Screening and Ruling out Active TB among HHCs of DR-TB Patients; Source: Guidelines for PMDT in India, 2021, p118.
Abbr: MDR/RR-TB: Multidrug-resistant/ Rifampicin-resistant TB; FQ: Fluoroquinolone; h: Isoniazid; R: Rifampicin; DR-TB: Drug-resistant TB; DS-TB: Drug-susceptible TB; TPT: TB Preventive Treatment; CXR: Chest X-ray; TST: Tuberculin Skin Tests; IGRA: Interferon Gamma Release Assay.
Salient Features of the Screening Algorithm
- Once a DR-TB patient is identified, all HHCs are counselled, screened and evaluated to rule out active TB.
- Nucleic Acid Amplification Test (NAAT) will be used up front among contacts with symptoms or abnormal Chest X-ray (CXR) to diagnose TB.
- If the result is Mycobacterium tuberculosis (MTB) detected with no resistance, the treatment for Drug-sensitive TB (DS-TB) is initiated.
- If the result is MTB detected with Isoniazid (H) and/or Rifampicin (R) resistance, manage as per DR-TB guidelines.
- If the result is MTB not detected, in HHC <5 years of age, assess for TB Preventive Treatment (TPT) and check for any contraindications.
- If the result is MTB not detected, in HHC >5 years of age with Latent TB Infection (LTBI) test positive or unavailable and CXR is normal or unavailable, check for any contraindications.
- If contraindications to TPT drugs exist, defer TPT and if no contraindication exists, offer TPT regimen as appropriate based on the Drug Susceptibility Testing (DST) pattern of the index patient
Follow-up for active TB as necessary, even for patients who have completed preventive treatment irrespective of TPT offer.
Footnotes
- HIV-positive contact: If <10 years of age, any one of current cough, fever, history of contact with TB, reported weight loss, confirmed weight loss >5% since last visit or growth curve flattening or weight for age <-2 Z-scores. Asymptomatic infants, <1 year, with HIV are only treated for LTBI if they are household contacts of a TB patient. TPT or Interferon Gamma Release Assay (IGRA) may identify People Living with HIV (PLHIV) who will benefit most from preventive treatment. CXR may be used in PLHIV on Anti-retroviral Treatment (ART), before starting TPT.
- Symptomatic HHC: Any one of cough or fever or night sweats or haemoptysis or weight loss or chest pain or shortness of breath or fatigue. Children <5 years should also be free of anorexia, failure to thrive, not eating well, decreased activity or playfulness to be considered asymptomatic.
- Other key and vulnerable population: Includes silicosis, dialysis, anti-TNF agent treatment, preparation for transplantation or other vulnerable risk groups where testing must precede TPT.
- Contraindication to TPT: Include acute or chronic hepatitis; peripheral neuropathy (if Isoniazid is used); regular and heavy alcohol consumption. Pregnancy or a previous history of TB are not contraindications.
- Selection of TPT regimen: Regimen is chosen based on considerations of age, strain (drug-susceptible or otherwise), risk of toxicity, availability and preferences.
- CXR may have been carried out early on as part of intensified case finding.
Resources
- Guidelines for Programmatic Management of Drug-resistant Tuberculosis in India, March 2021.
- WHO Consolidated Guidelines on Tuberculosis: Module 1: Prevention: Tuberculosis Preventive Treatment, 2020.
- Latent TB Infection: Updated and Consolidated Guidelines for Programmatic Management, WHO, 2018.
Kindly provide your valuable feedback on the page to the link provided HERE
Page Tags
Content Creator
Reviewer
Target Audience
- Log in to post comments