Content Status
Type
Linked Node
TB-Malnutrition: A vicious cycle
Learning Objectives-
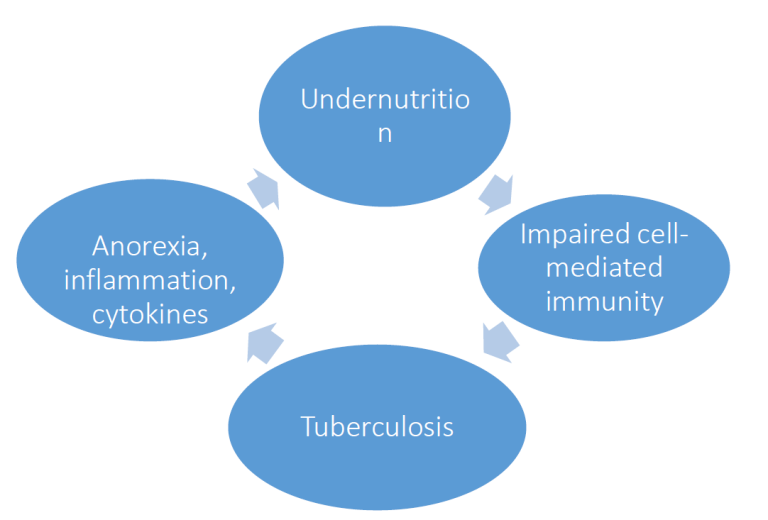
Fig. 1: The vicious cycle of undernutrition and TB and Undernutrition
Undernutrition can lead to progression of latent infection to TB. TB worsens undernutrition, which in turn increases the severity of TB disease. This is the vicious cycle of worsening disease and worsening undernutrition that needs to be addressed with nutritional support.
Effect of TB on nutritional status
TB is a disease classically associated with wasting, which occurs because of 3 mechanisms. The first is decreased intake because of anorexia and its
severity correlates broadly with the severity of clinical disease. TB increases the basal metabolic rate because of fever, although this increase is offset by the decreased energy expenditure due to decreased activity before the clinical improvement starts as a result of treatment. Finally, TB causes protein catabolism with a resultant negative nitrogen balance, with muscle breakdown under the influence of the acute phase response. In India TB occurs more often in the poor who are likely to have chronic undernutrition, food insecurity and more likely to encounter delays in initiation of
treatment. In such patients TB worsens the already poor nutritional status. Table 1 mentions the available data on dietary intakes, nutritional status and weight gain in patients with active TB in India. The available data suggests that dietary intakes are lower than those recommended for the age group, that Indian patients with TB are severely underweight at the initiation of treatment, when compared to the reference weights considered normal for Indian men and women (60 kg for men and 55 kg for women), and that weight gains are suboptimal. These mean body weights suggest that men and women are on average 28-30% below their respective reference weights. However nutritional recovery is possible with an adequate
balanced diet, as was seen in patients in the sanatorium group in the Madras trial, who received an adequate diet in terms of calories and proteins. The weight gain in these patients was 1.6-2 times that in the home group who were on the usual inadequate diet. The nature of weight gain is also important, and the aim of nutritional support should be to restore the lost lean body mass. Increase in weight due to increase in fat mass
will not improve functional status. However, it has been seen that patients whose intake of calories and proteins are normal, can regain lean body mass in a linear manner during TB treatment.
| Table1: Data on dietary intake, nutritional status and weight gains in TB patients in India |
| 1. Dietary intake Study in HIV positive patients with/without TB: 1546-2016 calories (Recommended population norm=2400 calories) |
| 2. Nutritional status of adult patients with active TB in India a. Data from NIKSHAY: Median weights in men= 43 kg Median weights in women=38 kg b. Large cohort from rural central India: Median weights in men = 42 kg, Median BMI in men=16.0 kg/m2 Median weights in women= 34.1 kg, Median BMI in women=15.0 kg/m2 53% of patients with MDR-TB under the PMDT had a BMI of less than 18.5 kg/m2 |
| 3. Weight gains in patients in India a. In the absence of nutritional support: RNTCP cohort: Mean weight gain =3.22 kg Non-RNTCP cohort(Rural central India) Mean weight gain= 3.9 kg (9). With nutritional support e.g. provided in the Madras trial Men: 7.8 kg (sanatorium treatment group) vs. 5.5 kg (domiciliary treatment group) Women: 11.0 kg (sanatorium treatment group) vs. 4.8 kg (domiciliary treatment group) |
| Prevalence of TB in India is higher in the lower socioeconomic status groups who are also more likely to have food insecurity. With the low baseline weights and suboptimal weight gain, many patients with active TB in India may not achieve nutritional recovery and are likely to be underweight at the end of treatment. |
Patients with active TB also suffer from micronutrient deficiency, esp. iron and folate, vitamin A, zinc, vitamin D. These micronutrient deficiencies are important as they can impair the cell mediated immune responses (e.g. zinc, vitamin D), anemia can impair quality of life and physical function. Seventy three percent of adults with active pulmonary TB in rural India had anemia, while in 20% the anemia was severe. The levels of some of the micronutrients can also be depressed by the acute phase response associated with active TB and can normalise at the end of treatment. Anti-TB drugs can also result in micronutrient deficiencies. For example, isoniazid administration can cause pyridoxine deficiency, and rifampicin can induce
metabolism of vitamin D and lower its levels.
Effect of nutritional status on risk and outcomes of active TB including drug-resistant TB
Undernutrition impairs cell mediated immunity which is critical for protection from active TB. Undernutrition is the most widely prevalent risk factor for development of TB in India and is a major driver of the TB epidemic in India contributing to around half of annual TB incidence in India. undernutrition in a patient with active TB is strongly linked to a number of adverse outcomes, and this deserves greater attention. Undernutrition can impair cell mediated immunity and increase the severity of TB disease. Moderate to severe undernutrition increases the risk of death related to TB and this is consistent in adults and children, in patients with/without HIV infection and in patients with drug susceptible as well as drug resistant TB. A weight of < 35 kg was associated with a nearly 4-fold risk of death in South India compared to weights more than 35 kg. The nutritional
status of patients is a strong predictor of treatment success in patients with drug resistant TB. In a recent study in a cohort of 330 patients with XDR-TB, the strongest predictor of unfavourable outcome was a weight less than 50 kg at the start of treatment. Undernutrition is also a risk factor for development of drug induced hepatotoxicity, which is a major side effect of anti-TB therapy, and this has documented in a number of studies in India. In one recent study, the risk of drug induced hepatotoxicity was 5 times higher in patients with a BMI less than 17 kg/m2. Drug induced hepatotoxicity can lead to treatment interruptions and default. Nutritional status can also influence drug pharmacokinetics and lower levels of some drugs like Rifampicin have been documented in undernourished patients in India. Undernutrition at diagnosis and inadequate weight gain during treatment, was associated with a 2- 4 higher risk of relapse in a trial. There is risk of TB among contacts of TB patients and food insecurity and undernutrition among contacts can increase this risk substantially. The weight gain in the initial few months of treatment has been noted to predict treatment outcomes. A weight gain of fiver percent after completing 3 months of treatment was associated with good outcome among patients with multi-drug resistant who were underweight before treatment. Therefore, nutritional support should aim at a weight gain of approximately 5% of body weight during the initial intensive phase of treatment.
Table 2: Effect of undernutrition on outcomes in TB
| Effects on disease : | Increased severity of disease Increased risk of death |
| Effects on treatment: | Delayed sputum conversion Risk factor for drug induced hepatotoxicity Malabsorption of rifampicin Reversion of positive cultures in MDR-TB |
| Effects on long-term outcomes: | Increased rate of relapse |
| Effects on contacts: | Increased incidence in undernourished contacts |
Resources
Assessment
| Question | Answer 1 | Answer 2 | Answer 3 | Answer 4 | Correct answer | Correct explanation | Page id | Part of Pre-test | Part of Post-test |
| Which of these is not a mechanism by which by which TB causes wasting? | Anorexia | Increased BMR | Protein catabolism | Low body nitrogen | 4 | 1,2,3 are correct answers | |||
| What effect does undernutrition have on TB treatment? | Delayed sputum conversion | Malabsorption of rifampicin | Drug induced hepatotoxicity | All of the above | 4 | All are correct |
Content Creator
Reviewer
- Log in to post comments