Content Status
Type
Linked Node
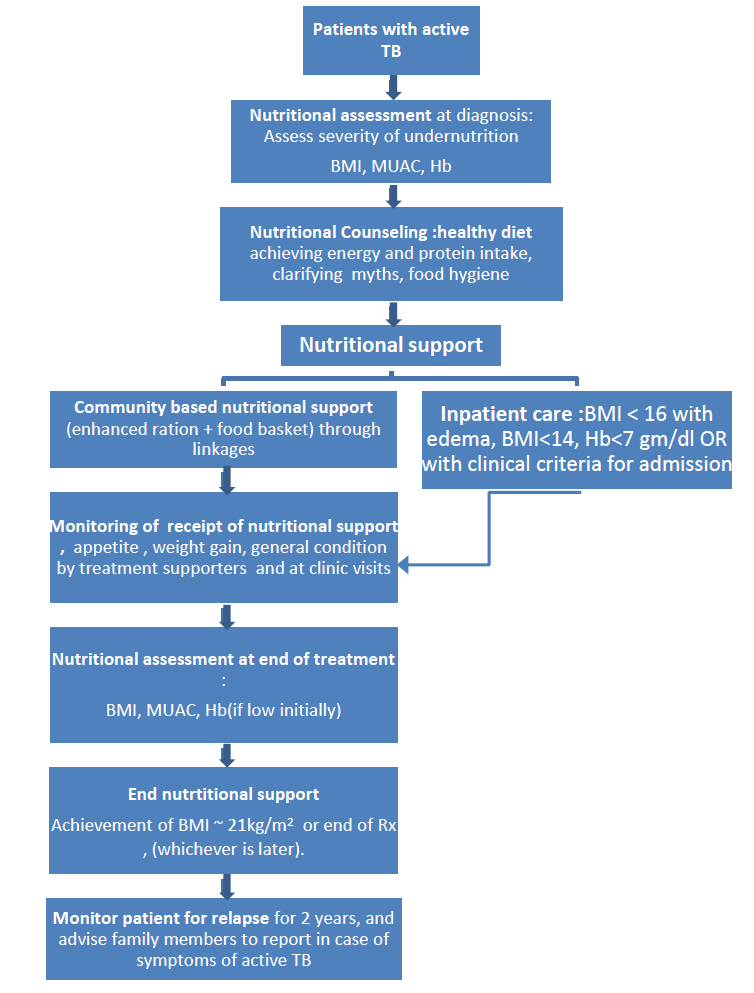
Pathway for Nutritional Management of patients with TB
Learning Objectives-
Nutritional assessment, counselling and support are now considered integral aspects of the care of TB patient. Therefore, these elements need to be integrated into the overall management of patients with active TB in India (including those with TB-HIV co-infection). India has the experience of conducting nutritional interventions on a large scale for certain segments of the population- there are supplementary nutrition programs for children between 6 months and 6 years, and pregnant and lactating women. There are nutritional rehabilitation centres for severely underweight children.
In addition to these, in view of the concerns of food insecurity, people below the poverty line have access to food grains at subsidized rates, across the country, under the targeted public distribution system (PDS) and Antyodaya Anna Yojana (AAY).
The working of the supplementary nutrition programs and the PDS differ from state to state in the amount of allocation of food grains, the foodstuffs distributed, and this has to be factored in the implementation of the nutritional support initiative.
Nutritional assessment
At treatment initiation, the treating doctor should take note of the height and weight of the patient. If the patient is a child then z scores of weight for height, are useful to determine the nutritional status. If the patient is an adult and is unable to stand then the MUAC may be recorded. These measurements can be done by the staff nurse at the healthcare facility. In the case of children and adolescents, the charts of weight for height and BMI for age will be consulted by the physician/paediatrician to determine the severity of undernutrition. The assessment of vital signs in patients
may indicate need for inpatient care. As discussed earlier, patients with extremely low BMI (BMI < 14 kg/m2) will need admission for stabilization, inpatient care and initiation of nutritional support to an appropriate healthcare facility, where specialised in-patient care can be provided.
Nutritional counselling
This will involve assessing the current dietary intake of the patient, the dietary preferences and discussing the appropriate diet in terms of composition, frequency of meals and snacks. The patient will be advised on how to use to increase the calorie and nutritional density of locally available foods. The family members of the patient will also be explained that the nutritional supplement (milk powder, groundnuts, pulses) are a kind of medicine for the patient in order to ensure recovery of the lost weight and muscle mass, and that the supplement should be primarily be consumed by the patient.
Nutritional support
Resource mobilization
Many states have demonstrated successful models on a small scale.
a. Local Self Government initiatives. The three tier Panchayati Raj system has provided ample opportunities for decentralized planning and implementation of developmental projects. Nutritional support to TB patients may find place among the annual projects of district/block/gram panchayats with appropriate estimates of budgets considering the annual TB notification, proportion of cases that would require additional nutrition and cost of food basket with locally available ingredients.
b. Corporate Social Responsibility (CSR): There are some successful initiatives utilizing CSR funding for nutritional support to TB patients. This has a role especially in piloting new strategies for certain defined population, eg- miners, urban slum population, certain tribal areas etc. However expandability and sustainability of these initiaves need to be planned carefully.
c. Intersectoral collaboration. Many state government departments are implementing various support including nutritional support to citizens generally or to patients suffering from specific diseases. Since the beneficiaries and often the providers are not aware about these supports, public resources for the same are not being effectively utilized. Some of these schemes are monitory, these could be pooled and converted to nutritional support.
Procurement of food baskets for patients
a. Linkage with the public distribution system: A state/Panchayati Raj Institution may coordinate with the PDS for procurement of these food items.
b. Procurement and delivery of these food items may be done by NGOs under a scheme evolved for this purpose.
Delivery of enhanced ration through linkage with the public distribution system
An enhanced PDS ration needs to be provided for the duration of anti-TB treatment along with a supplement food basket. Most of the patients who develop active TB are likely to have a BPL card which will enable access to an enhanced ration (double the usual allocation) through the targeted PDS system. It is expected that state 66 Departments of Health and Family Welfare establish linkages with the Department of Food and Civil Supplies at all levels. Necessary Government Orders may be issued in this regard to the functionaries of both departments. Program staff and healthcare staff need to facilitate the dissemination of nutritional support guidelines and supportive Government Orders down to the most peripheral level of PDS distribution. Diagnosis of TB makes the BPL patient eligible for a double ration. However if the patient does not have a BPL card, it is recommended that a card be issued to the patient and his family which shall cover the duration of the treatment. Necessary clauses to this effect may be included in the GOs. Alternatively, food vouchers could be evolved which can enable the patient to access an enhanced PDS ration. In case of beneficiaries of the Antyodaya Anna Yojana, an additional 10 kg of foodgrain could be made available in addition to the supplemental food basket. Once a TB patient is diagnosed, the PHI Medical Officer may certify that the patient is eligible for a double ration. In the case of both the BPL and APL patients, the local
PDS distributor should be able to take the decision to provide the support. Coordination between the programme and the PDS system authorities will prevent any delay in initiation of food support.
Delivery of supplemental food basket: available options
Food items like milk powder, groundnuts, are not routinely distributed through the PDS outlets. The delivery of the supplemental food basket may be entrusted to NGOs under a scheme evolved for this purpose. The patient may verify the delivery of the food items in this model. Food vouchers is another option, with which patients can access defined food items from neighbourhood shops
NGO Scheme for nutritional Support to TB patients
Suitable schemes may be developed for providing nutritional support to patients in line with existing other schemes for engagement of NGOs.
Inpatient nutritional support and care
The inpatient facility at a community health centre or of a district hospital/medical college can serve as the point of care for a patient with Severe Acute Malnutrition and active TB. This is being recommended as the investigations (electrolytes for example), as well as specialist staff are available at the CHC. Once the patient recovers his/her appetite and starts gaining weight the patient may be followed up at the PHC level.
Social support as part of patient-centred care
Social support as part of patient-centred care is needed to ensure long-term food security for patients and households suffering serious and catastrophic consequences. Some families of patients with TB suffer serious consequences as a result of the disease and its sequelae, which have short as well as long term impact on their food and income security. The new End TB strategy emphasises patient centred care and provision of social protection measures. According to the International Labor Organisation these measures comprise access to essential social services and social transfers including in cash and in kind paid to the poor and vulnerable to enhance food security and nutrition, provide a minimum income security and access to services, as well as income replacement and social support in the event of illness. Some illustrative examples of these serious situations are listed below:
- Death (especially premature) of any of the parents during TB treatment
- Occurrence of TB in more than one member of the family, which can be especially serious in the case of MDR-TB
- Severe disability due to TB: This is usually a result of extensive pulmonary TB with extensive fibrosis which may not allow a person to return to his usual occupation. However, TB meningitis, intestinal TB, bone and joint TB, pericardial TB may also cause disability, which may be serious or permanent
- Occurrence of TB, or TB death secondary to silica exposure at work
- Catastrophic costs resulting in loss of assets like land.
Such situations may come to the knowledge of the treatment supporter, or the field level supervisor. Knowledge of some of the social sector schemes might help the programme enable the access of the patient’s family to these schemes. E.g. in the case of death, the family is eligible for assistance of Rs. 20,000 under the National Family Benefit Scheme, or in the case of patients dying of silico-TB, a compensation of Rs. 3 lacs has been enforced by the Government of Rajasthan. These schemes are listed in annexure 10 of the Guidance document nutritional care and support for TB patients in India. Across India for certain population groups like persons belonging to scheduled castes and scheduled tribes are provide financial and nutritional support on the initiative of local developmental agencies e.g. Integrated
Tribal Developmental Agency. Such situations can also be documented by the programme and an effort can be made for provision of social support through other channels – e.g. corporate social responsibility initiatives.
Nutritional monitoring, recording and reporting
Response to nutritional replacement may be assessed by serial documentation of weight, changes in appetite and degree of independent activity. Patients, who do not display weight gain, continue to be anorexic and are unable to perform basic daily routine activities may be considered to have failed to respond to nutritional therapy. Failure to respond to treatment in adults is usually due to an unrecognized underlying illness (see page 37), a nutrient deficiency or refusal to follow the treatment regimen.
Follow-up phase
In the follow up phase which may last up to 6 months the patient is monitored in the progress towards normal nutritional status which may be recorded in a suggested NTEP register for patients receiving nutritional support (annexure 11). Since a number of studies have documented a higher risk of adverse outcomes during and after treatment with a less than 5% weight gain in 2 months, this is the minimum desirable weight gain in the first 2 months. A 10% weight gain in 3 months would be optimal. The target body weight in a patient varies according to the height of the patient and will correspond to one which correspond to at least a BMI of greater than 18.5 kg/m2 or ideally will correspond to a BMI of around 21 kg/m2 ( see box below) Document weight and appetite at each outpatient visit.
| Weight gain to be achieved during therapy: An example (annexure 9) If the patient has a baseline weight of 40 kg and has a height of 160 cm. Then the baseline BMI is 15.62 kg/m2, which indicated severe undernutrition. The patient should gain at least 10% of his body weight in 3 months i.e. a gain of 4 kg in 3 months, of which at least 2 kg should be in the first 2 months. The minimum desirable body weight in the patient corresponding to a BMI of 18.5 kg/m2 in this patient will be equal to 18.5 x (1.6)2= 47.4 kg An optimal body weight in this patient which will correspond to a BMI of 21 kg/m2 would correspond to a weight of 21 x (1.6)2= 53.8 kg. |
A limited number of observations and tests from the table below may also be performed. Other associated abnormalities documented during admission such as anemia must be reviewed on an outpatient basis till normal.
Follow up monitoring
| Parameters | Frequency of observation by healthcare staff |
Rationale |
| Anthropometric | ||
| Weight /weight for age | Monthly or at least on 2,4,6 months |
The nutritional improvement can be documented and troubleshooting done. |
| BMI/BMI for age | Monthly or at least on 2,4,6 months |
|
| MUAC | Monthly or at least on 2,4,6 months |
|
| Clinical condition | ||
| Fever , cough | Weekly by treatment supporter then monthly |
To document clinical improvement and refer if failure to response |
| Appetite | Weekly by treatment supporter then monthly |
To document clinical improvement and refer if failure to response |
| Edema | Weekly by treatment supporter then monthly |
To document clinical improvement and refer if failure to response |
| Breathlessness | Weekly by treatment supporter then monthly |
To document clinical improvement and refer if failure to response |
Nutritional outcomes and their recording in patients
Discharged/cured: Weight for height scores > -2 z- scores (for 6 -59 months), BMI for age > -2 z-scores for age. BMI for adults> 18.5 kg/m2 in 2 successive visit.
Non-cured: Absence of weight gain of 10% of baseline weight in 3 months
After the end of treatment patient and his/her family must be followed up for symptoms including weight loss 2 more years for early detection of relapse.
Resources
Assessment
| Question | Answer 1 | Answer 2 | Answer 3 | Answer 4 | Correct answer | Correct explanation | Page id | Part of Pre-test | Part of Post-test |
| What is the minimum desirable weight gain in the first 2 months of treatment in TB patients? | 10% | 5% | 3% | 12% | 2 | 5% is the minimum desirable weight gain in the first 2 months. A 10% weight gain in 3 months would be optimal | |||
| Ideally, how often should and weight, BMI and MUAC be measured for TB patients under treatment? | Monthly | Bimonthly | Monthly in intensive phase and bimonthly later | Every fortnight | 1 | Ideally, anthropometric measurements may be taken monthly but at least on 2,4,6 months. |
Content Creator
Reviewer
- Log in to post comments