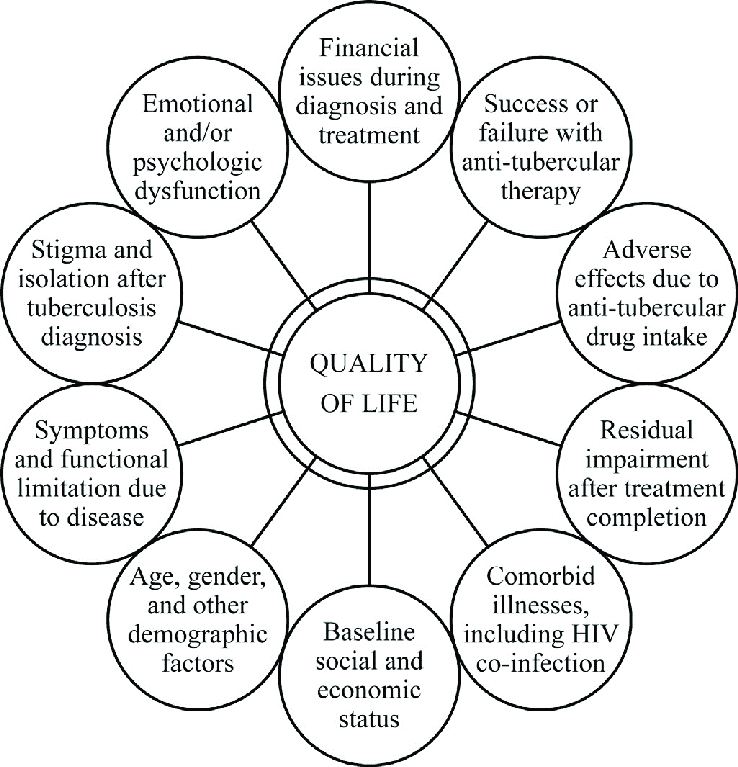
The suffering faced by people with TB and their families may be due to the disease itself, the treatment, co-morbidities and adverse outcomes of anti-tuberculosis drugs. Suffering in TB is multidimensional affecting physical, psychological, social and spiritual domains of the person. Thus, palliative care has a major role in TB and must be integrated into the course of TB care. Every person with TB should be motivated to continue and complete anti-tubercular treatment. For people affected by TB with complex physical, psychosocial or spiritual needs, palliative care should be considered early in the course of illness, in conjunction with disease-directed treatment.
1.Aim of providing palliative care to people with TB
The problems faced by people with TB3 and families span multiple physical, psychological, social, and spiritual dimensions. Palliative care is an approach that improves the quality of life of people with TB and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment and treatment of physical, psychosocial or spiritual problems. The aim of palliative care in TB4 should be alleviation of sufferings caused by the primary disease as well as adverse effects of the anti-tubercular drugs to improve the quality of the life during and after completing TB treatment with provision of end-of-life care when required. Integration of palliative care improves treatment outcomes by enhancing treatment adherence and also prevents premature deaths.
2.Key population for providing palliative care
Specific groups who will definitely have increased palliative care needs include those with drug resistance5 (MDR/RR-TB, Pre-XDR/XDR-TB), who are co-infected with HIV, those having severe disease including multi-organ involvement or failure, those with severe forms of extra pulmonary TB and those with recurrent/chronic TB.
Apart from this, there is another group of people who get microbiologically cured but are left with Post TB sequalae also called Post TB Lung Disease (PTLD) including destroyed lung, Fibro cavitory disease, Aspergilloma, Bronchiectasis etc. Up to 50% of people with microbiologically cured TB may be left with permanent, moderate or severe pulmonary function impairment; experience exercise limitations and have a hampered quality of life. This group of people finally land up in Respiratory failure and may require long term care.
3.Challenges in providing palliative care to people with TB
PMDT guidelines 2021 outline the need for palliative care in TB and mandate the Nodal TB Centers to initiate institution-based and community-based palliative care services. Through NTEP, many aspects of palliative care are covered in different forms like home visits by TBHV, counseling by TB counselors, nutritional support through Nikshay Poshan Yojana, peer support through TB champions, community support in the form of Nikshay Mitra, travel allowances, Pradhan Mantri TB Mukt Bharat Abhiyan (PMTMBA) etc. However, palliative care for people with TB and their families remains underdeveloped.
There are two main barriers to advancing the availability of palliative care for TB. Due to the curable nature, there is some inherent resistance to the idea of palliative care for people with TB. The second main barrier is simply the lack of knowledge of palliative care principles and practice among the providers who care for TB.
4. Special considerations for providing palliative care to people with TB
●Large number of people requiring palliative care in TB is infectious, so airborne infection control practices need to be strictly followed.
●People with post TB lung disease (PTLD) may not be contagious (bacteriological evaluation of sputum to be done to rule out active disease) but have significant lung damage in the form of Destroyed lung, Bronchiectasis, Aspergilloma and land up into Type II Respiratory failure over a period of years. Such a group of people can be taken care of by home based palliative care type of model, as they are not contagious
●People with PTLD with compromised lungs may suffer from other health related issues: symptomatic cholelithiasis, symptomatic nephrolithiasis, hernias and require corrective surgeries; but are not taken up for surgeries as may not be fit for anesthesia due to compromised respiratory system. Minimal access surgery options should be incorporated in palliative care services.
●People with recurrent Drug sensitive or Drug Resistant TB with localized disease are eligible candidates for surgical resection of the affected part but are not considered for due to their microbiologically positive status. Moreover, people with DSTB or DRTB who suffer from other surgical problems and need immediate surgeries to relieve the suffering are not entertained just because of their bacteriologically positive status. A guidance document on indications for TB thoracic surgeries and capacity building of surgeons in this regard is required.
● Though dyspnea is the dreaded symptom in extensive PTB and in the majority of people with TB at the end of life; still, TB facilities have limited access to opioids. In low doses, morphine suppresses the respiratory center slightly and has an anti-anxiety effect. This relieves tachypnea, increases tidal volume and oxygenation. Thus, low dose morphine increases effectiveness of respiration in people with hypoxia. Additionally, it also relieves pain. TB institutions with high patient load and providing palliative care need to have access to opioids.
5. Palliative care models for various key population affected by TB
|
Key Population |
Recommended palliative care model |
|---|---|
|
Newly diagnosed microbiologically confirmed/clinically diagnosed TB
|
Integrate palliative care into the package of essential services for TB, prioritizing those individuals who need it. |
|
People with Post TB sequelae |
Traditional Home care-based model along with hospital-based care as and when required |
|
People with recurrent Drug Sensitive TB and Drug Resistant TB |
Hospice based model on the lines of traditional sanatorium-based care along with special consideration to take care of caregivers and infection control measures |
“There is no single recommended model for the provision of palliative care; the best model is determined by local needs and resources
Figure 1 – Ensuring the continuum of Palliative care services for TB7 (adapted from WHO guidelines for Palliative care)
- Printer-friendly version
- Log in to post comments